
The Supreme Guide to LPR Causes & Treatment
There are many causes of LPR.
Which is why there are many potential solutions as well.
Many physicians treat generically – each patient receives the same treatment. If the patient is lucky, that treatment tackles the root cause. If not, the LPR symptoms will persist or come back.
For a permanent cure, you need the right solution for your individual problem.
Let’s have a look at 5 groups of LPR contributors and their respective treatment:
LPR Treatment: Common Causes and their Fixes
1. Weak Sphincters
The key contributor to laryngopharyngeal reflux (LPR) are malfunctioning sphincters.
Sphincters are valves that keep food in the right organ of your digestive system until it’s ready to be passed on.
Whenever one or more of those sphincters do not work as they should, problems start to happen – often in the form of reflux.
These are the three sphincters that play a role in LPR:
A) Lower Esophageal Sphincter (LES):
The LES is the first anti-reflux barrier and the best-understood sphincter. It sits directly above the stomach.
The LES has a complicated task. It needs to open at exactly the right moment. Only then is it possible to swallow food, yet still prevent reflux the rest of the time. For reasons not yet completely understood, the LES relaxes regularly. Those events are called transient lower esophageal sphincter relaxations. Maybe it is a way to relieve pressure in the stomach.
Everybody has these relaxations which is why everybody also has reflux. The point is: People with reflux symptoms have those relaxations more often. Your body can tolerate some reflux. Only when it becomes too much, you start to feel the symptoms.
The lower esophageal sphincter is a muscle. However, it works differently than most muscles in our body. It does not get stronger if we use it a lot – it gets weaker! It is a little bit like when you have back pain from sitting too long in one position. You are overusing some muscles. But instead of becoming stronger they become tense and painful. They stop fulfilling their function as they should.
The lower esophageal sphincter reacts in the same way if it is being put under unnatural stress for long periods of time. It becomes unable to fulfill its function as a barrier against reflux.
After years of overeating and late night eating, the lower esophageal sphincter can get weaker and reflux can increase. Most people do not even realize that they are eating unnaturally – as pretty much everybody these days is doing it. We grow up with it.
How to Treat a Malfunctioning LES
Diet
It will have a high impact if you start eating smaller meals. That will put less stress on your LES.
Even more important is to stop late night eating. As long as you are in an upright position, gravity is on your side. When you lie down, the contents of your stomach are pressing on the LES. On top of that, digestion is slower when you sleep. While most people with LPR reflux during the day, the worst cases are due to nighttime reflux. At night, all of your anti-reflux defenses slow down, which is why reflux causes more damage.
There are some foods that impair the function of the lower esophageal sphincter. Some relax the sphincter-like chocolate, caffeine (coffee, tea, etc.) & alcohol. Others produce gas which presses open the sphincter, like onions. I will talk more about diet later in this article.
If diet alone is not enough, there are also surgeries available:
Surgery
A very established surgery is the Nissen Fundoplication in which a part of the stomach is wrapped around the LES to tighten it up.
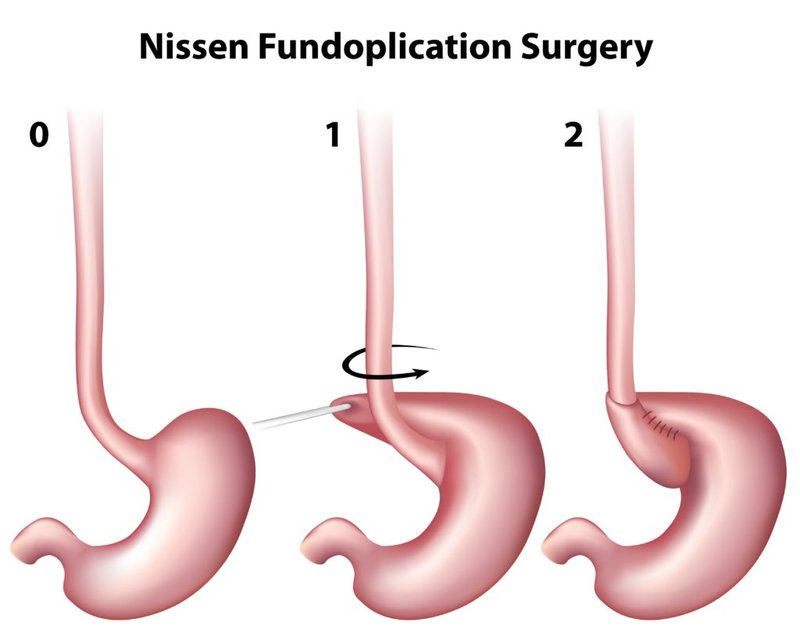
The Fundoplication is proven to work for most LPR patients. However, side effects like bloating are common and can be severe. Also, it is a permanent option. You can redo it if the wrap loosens up. You can have it loosened to relieve side effects. But you are going to be stuck with a fundoplication for life.
A newer solution is the LINX device. It is a band of magnetic beads which is implanted around the lower esophageal sphincter. The upside of the LINX is that it can be removed if it causes problems. However, there is very little data on how well it works for LPR patients. Most experts recommend the Nissen Fundoplication over the LINX.
I think another surgery will be the first line of defense against LPR in the future: the Stretta Procedure.
The procedure is fairly new, a bit more than 10 years old. It takes longer for standard medical treatment guidelines to change. While Stretta is less effective in fighting reflux than other procedures, it is low-invasive and rarely has long-term side effects.

When you do a Stretta, the muscles of your LES are stimulated with electricity. This causes them to grow and reduces the amount of relaxations. The downside is that it takes a few months after the treatment to feel the results. That is how long it takes the body to build more and stronger muscle.
The good thing with Stretta is, if you do not get better, you can still do any other kind of surgery. The Stretta does not cause conflict with other procedures as it only grows muscle and improves its behavior.
Medication
There is medication which can increase the pressure of the sphincter, for example so-called prokinetic agents. Another agent is Baclofen which reduces the frequency of sphincter relaxations. The problem is that all those agents can have significant side effects – psychological, neurological and on the motoric function - which is why they are rarely used.
Medication can be great to assist with the healing process in the short term. Patients who need them long term are usually better off with surgery. The risk/benefit ratio is simply better.
It is important that your LES can resist the pressure in your stomach. The lower esophageal sphincter is the first line of defense against laryngopharyngeal reflux.
The more reflux gets through, the more the next barrier, the upper esophageal sphincter, has to fight.
B) Upper Esophageal Sphincter (UES):
The UES is the final barrier before reflux reaches your airways.
If your UES malfunctions, you will develop LPR symptoms.
The airways have minimal resistance to reflux. They can be damaged by amounts of reflux that the esophagus would not blink an eye about. That is why many people have LPR but no heartburn.
Despite the UES’ importance in LPR, there has been little research done on it. That is because up until recent years LPR did not get much research attention.
How to Treat a Malfunctioning UES
The UES often recovers through a better diet alone.
LPR is a vicious circle.
The tissue that lines the UES becomes inflamed which reduces the sphincter’s ability to function. This creates even more reflux. Reducing the reflux with a proper anti-reflux diet can break the vicious circle.
C) Pyloric Sphincter
The pyloric sphincter sits in between the stomach and the intestines. It's job is to keep food in your stomach until it is digested enough to travel forward.
Problems start if your pyloric sphincter is stronger than the LES above your stomach. For digestion to work, your stomach needs to contract and press food out into the intestines. If the LES is weaker, it will open up instead of your pyloric sphincter.
Imagine it like a tube of toothpaste. Usually, when you press the tube, the paste should come out of the opening in front. Now imagine you cut a big whole into the back of the tube. When you press, the paste suddenly comes out both openings. The same happens in reflux. If the LES does not hold tight, there will be two openings for food to leave the stomach.
One reason for a malfunctioning pyloric sphincter is that the supplying vagus nerve is damaged. It is not that uncommon.
The result can be delayed gastric emptying (gastroparesis) with symptoms like bloating. Your stomach can not empty itself properly as parts of the gastric content are pushed into the esophagus instead of the intestines. According to Dr. Mark Noar, up to 40% of people with reflux have this problem.

A malfunctioning pyloric sphincter can be diagnosed by doing an electrogastrogram (EGG). The test senses electrical signals that are coming from the muscles of the stomach. It is a similar test to an EKG that is used to evaluate the function of the heart.
How to Treat a Malfunctioning Pyloric Sphincter
It is possible to dilate the pyloric sphincter while doing an endoscopy of the stomach.
However, it is a procedure that is still rarely done for reflux patients. Probably because the knowledge about pyloric sphincter malfunction and its treatment is still rather new and not widespread.
2. A Common Mistake: Acid
Acid causes reflux. Or maybe not?

Well, “normal” reflux is caused mostly by acid, yes. With normal reflux, I mean symptoms in your esophagus like heartburn.
However, with LPR, acid is only a part of the equation. Much more important is to understand the role of pepsin:
3. Why Pepsin Plays a Crucial Role in Curing LPR
LPR is caused by a combination of acid and the stomach enzyme pepsin.
The job of pepsin is to digest proteins in the stomach. If you have LPR, pepsin gets up into your throat and airways. There it goes on with its job: digesting. It’s just that pepsin now digests the cells of your airways. That does not sound good, does it?
Pepsin is highly influenced by the presence of acid.
The acidity is expressed by the pH. A pH of 1-2 is about the level of the empty stomach and is very acidic. A pH of 7 is neutral. Everything above is alkaline.
Usually, the pH in the throat is about neutral. Pepsin becomes inactive in such an environment. However, each time pepsin comes in contact with acidity, it becomes reactivated.
The lower the pH is, the higher the damage potential of pepsin:

Once refluxed, pepsin can stay in your airways for days or weeks.
What You Can Do About Pepsin
It is crucial to avoid drops in acidity in the throat and airways. Otherwise, the damage potential of pepsin will be increased massively.
One way to do that is to avoid reflux in the first place. For example, by fixing your sphincters which we already talked about above. Each acidic reflux will not only transport new pepsin into the throat, but on top of that, the acidity will reactivate the pepsin that is already there.
Other treatments target pepsin more directly:
Avoid Acidic Drinks & Foods
Each time you consume acidic drinks or foods your throat is bathed in acidity. It will reactivate pepsin and promote LPR symptoms over time.
Dr. Jamie Koufman is a pioneer in low acid diets to treat the symptoms of laryngopharyngeal reflux disease. She wrote a whole book on how you can control LPR with diet, especially by removing acidic foods and drinks.
According to her, anything under pH 5 should be banished from the diet, at least until the symptoms have disappeared. After that, a cautious reintroduction of slightly acidic foods up to pH 4 is possible.
Almost all fruits are more acid than pH 5 and therefore not a good choice for LPR sufferers.

Sodas like cola and Fanta are even more acidic than most fruits. Sodas are about as acidic as lemons. Their pH is between pH 2.5 and pH 3. The sugar in soda is covering up the acidic taste. Without the sugar, sodas would be inedible.
Melons are an exception. They have an about neutral pH and can, therefore, be eaten.
You have to be careful when you are looking up the acidity of foods on the internet.
In LPR, it is relevant which pH food has when it passes through the throat. This is the moment when acids can reactivate the pepsin and cause them to destroy the mucus membranes. However, many sources on the internet refer to whether acids or bases (alkaline substances) are formed during the metabolism – meaning inside your body. Pepsin does not care about what happens after digestion. However, it is of relevancy in some diseases like arthritis which react negatively to acidity in the body. Much data on the Internet references those values AFTER digestion.
I know this is confusing. If in doubt, you can test the pH of foods with pH strips. I also have an extensive list of the acidity of foods and drinks in my online course.
Alkaline Water
While acidity reactivates pepsin, alkalinity above pH 8.8 permanently deactivates pepsin. That means afterward, even acidity can not make the pepsin work again.
Drinking or gargling with alkaline water is helpful for “washing” the pepsin out of your throat. This is not a miracle cure. You will only be able to hit pepsin in your mouth and throat. Some of the water will also spill through the entrance of your larynx.
Alkaline water can be one step in the direction of symptom resolution. Just keep in mind that alkaline water cannot do anything against you refluxing new pepsin. You still need to fix the reflux itself.

Some people show improvement by drinking or gargling alkaline water while others show no improvement at all. You have to try it out.
There are multiple ways to get or make alkaline water:
Bottled: Some brands like Evamor are naturally alkaline. It is the healthiest solution – but also the most expensive.
Baking Soda: You simply mix it with water. You can get baking soda everywhere that sells baking supplies. The chemical name is sodium bicarbonate. It a substance which is natural in your throat. It is excreted by the mucosa to neutralize acid. That makes it part of your natural reflux defenses.
Baking soda is very cheap and easy to transport.
The problem with this solution is that you will consume loads of sodium which is not good if you have problems with high blood pressure. It can also lead to side effects like water retention & edema when you overdo it.
On the other hand, some people say that you specifically need sodium bicarbonate to permanently deactivate pepsin. Baking soda is pure sodium bicarbonate.
pH Drops: There are bottles that contain concentrated alkaline minerals which you can use to make any water alkaline. Often they are sold under names like "pH boosters". You just place a few drops in a glass of water. While they definitely increase the pH I am not sure if they make a difference with LPR. It has been suggested by me by Dr. Mark Noar that it might actually be a chemical reaction caused by the bicarbonate that deactivates pepsin - not just any high pH level. Those pH drops contain different minerals (usually not bicarb) and might not help at all. They also become expensive very quickly with regular use.
Other Solutions: There are different machines and water filters that promise to create alkaline water. Those machines can be a very expensive investment. On the other hand, they might come out cheaper than the other solutions if you use them for years. I have never tested any of those machines so I cannot tell which ones are good.
If you make your own alkaline water, you will need pH test strips (like the ones I mentioned above) to make sure your solution has the right pH. I recommend targeting pH 9. Producing your own alkaline water is never completely exact. If the water is in the range between pH 8.8 and 10 it should be fine. Do not go higher as it will lead to new problems like high sodium levels or neutralizing the acid in the stomach which you need for digestion.
I gargle with alkaline water in the morning (my reflux is nocturnal) and drink a few sips. That way I harness the upsides of alkaline water while minimizing the downsides.
Why PPIs are a Usually a Poor Treatment Choice
Many physicians ignore the role of pepsin in LPR and only treat the acidic component. That is why acid-reducing medication does not work well against LPR.
The most commonly prescribed medication to reduce acid production is a group of drugs that are called proton-pump inhibitors (PPIs). They are very effective at reducing the acid output of your stomach.
Here are the brand names of the available PPIs and in brackets their generic names:
Nexium (Esomeprazole)
Prilosec (Omeprazole)
Prevacid (Lansoprazole)
Dexilant (Dexlansoprazole)
Protonix (Pantoprazole)
AcipHex (Rabeprazole)
Studies Show: PPIs do not Work for LPR
Proton-pump inhibitors are prescribed like crazy for LPR. That is insane, considering that numerous studies have shown they do not work for this type of reflux.
You might ask, why do PPIs not work? After all, we already established that acidity causes pepsin to be more active. Wouldn’t that mean that PPIs should help as they reduce the acidity in the reflux?
Most studies only show the average improvement of all patients in a study. A theoretical example: If half of the people get 30% better and the other half gets 30% worse, the study will show that the medication did not change anything – on average. Improvement and damage nullify each other.
From feedback of patients and physicians, I assume that some people indeed get better on PPIs while others get worse. Why people can get better on PPIs is easy to understand: less acid in the reflux means pepsin is less active & harmful.
However, the side effects of PPIs include numerous negative gastrointestinal symptoms. Anything that puts the digestive process out of balance might also lead to more reflux.
Additionally, the acid usually dilutes the pepsin in the gastric content. If you block acid production, it means that the concentration of pepsin in the reflux is higher.
An additional theory sees gas-producing bacteria as a cause of reflux. The bacteria consume incompletely digested food and emit gas. PPIs might lead to more incompletely digested food and therefore more gas. We will talk more about that below.
All of those (potential) negative effects of PPIs might cancel out the benefit of taking acid blockers and therefore explain why studies fail to show benefits of PPIs against LPR.
However, this also means that when we look at single individuals, PPIs might be beneficial. Experts that I trust recommend them in combination with a silent reflux diet – but only in selected patients and only for a few weeks or maximum months. PPIs – especially in long term usage – can create new gastrointestinal disorders which kick you into a vicious circle.
Be Careful of Overly Eager PPI Prescribers
What I hear from most of my readers is that their physicians prescribe completely contrary to that. They prescribe PPIs to LPR patients like tic tac's.
It is a bit perverse that many medical recommendations for physicians say that if PPIs do not work for a patient after one month, they simply should be prescribed for 3 months – and then for 6 months if that still fails. Instead of changing the approach, something that did not work in the first place is simply tried again and longer.
I guess the pharmaceutical companies who produce proton-pump inhibitors had a strong influence in creating those recommendations.
PPIs are earning billions of dollars for the pharmaceutical industry every year.

It plays into the hand of big pharma that most physicians are unaware of the latest research about the role of pepsin in LPR. Those physicians think that blocking the acid production will work for LPR as it does for reflux into the esophagus (GERD). It is not correct but an understandable assumption.
In the past, I used to do market research for pharmaceutical companies by interviewing physicians and pharmacists to analyze their knowledge.
I learned that not all, but many companies will use a lack of education about a disease to their advantage where they can – in this case, to push more PPIs against LPR onto the market. That is why I got into the education of people instead of doing market research.
Rebound Effect – Increased Reflux Symptoms after PPIs
If physicians do not specialize in LPR, I strongly recommend to question when they try to put you on PPIs – especially as it is tough to get off them. The longer you take PPIs, the stronger the reflux symptoms become once you stop taking them.
This phenomenon is called the rebound effect. Not only reflux sufferers have worsened symptoms when stopping PPIs usage. Even about half of healthy people will get heartburn symptoms if they have taken PPIs for one month and then stop taking them.
The longer you have taken PPIs, the longer it will take for your acid production to go back to normal.
Taking PPIs for just 2 weeks would be not a big deal. But for LPR most physicians prescribe PPIs for much longer.
I get emails nearly daily from readers who have been prescribed PPIs for 4-6 months. Many of those patients do not get any improvement on the PPIs. However, they struggle to stop taking them as they get worsened LPR symptoms or heartburn.
I do not want to tell you that you should not take PPIs at all. What you should understand is that PPIs are prescribed like tic tac’s - - without a good understanding of their limited potential to treat LPR.
There are also H2-Inhibitors, also called H2-Blockers as a type of acid reducing medicine. Examples are Zantac (ranitidine), Pepcid (famotidine) and Tagamet (cimetidine). They are less effective in reducing acid production than PPIs, at least on an empty stomach.
H2-Inhibitors have limited use in LPR for the same reason as PPIs. They have fewer side effects than PPIs. The reason is that H2-Inhibitors are weaker than PPIs and do not reduce acid production as much. Compared to PPIs, they do not produce rebound effects – or only light ones.
If your stomach is empty, H2-Blockers work better than PPI which is why they are often prescribed for during the night.
Gaviscon Advance
Gaviscon Advance is a pharmaceutical product from the UK. It contains an algae extract. After swallowing, it creates a foam on the surface of the gastric content.
This foam acts as a barrier which keeps the stomach content where it belongs. Additionally, the algae extract filters the reflux by binding pepsin. That means less pepsin will make it into the airways. The effect of the filter will be strongest shortly after taking Gaviscon Advance and wear out over a few hours.
Gaviscon Advance won't stop all your reflux or pepsin from coming up. But it makes an observable difference in many patients. Studies have shown that Gaviscon reduces LPR symptoms much better than placebo.
Attention: Gaviscon Advance is not available in the U.S. The Gaviscon product there is a simple antacid that does not work against LPR.
The U.S. Gaviscon contains no alginates and therefore has neither barrier effect nor filters pepsin.
While you cannot buy Gaviscon Advance in the U.S., you can buy it from importers on Amazon.
4. Can Low Stomach Acid Cause LPR?
The internet is an amazing tool to find information on improving your health.
The downside is that there is information which sounds very accurate, but is actually incorrect. The reason is that many websites are financed by advertising. Most forms of online advertising only pay a few cents per reader. To make the business model work, publishers hammer out a huge mass of articles - often on multiple websites. The quality of those articles is secondary.
Of course, there are sources of high-quality information out there.
However, it can be difficult to decide which advice is legit and which not.

I get emails all the time asking me why I do not write more about the “true” cause of reflux: low stomach acid.
Many people in online forums, less well-researched health blogs, and the social media are raving about how you supposedly can heal reflux by supplementing with artificial stomach acid to boost your digestion. Most people I know who tried that only got a painful stomach (gastritis) and sometimes worsened reflux symptoms.
All this buzz around low stomach acid started with Jonathan Wright’s book about “Why Stomach Acid Is Good for You”. The book describes exhaustively how acid and digestive enzymes are the basis for healthy digestion – which is correct.
An assumption of the book is that low stomach acid is the root cause of many diseases, also of reflux. Wright makes it sound like he can heal nearly any refluxer by boosting stomach acid.
The author is right that stomach acid is crucial for long-term digestive health. A very small percentage might even get reflux from it.
However, there is no data that shows this being the case for most people. If low stomach acid is so common in reflux patients, it would be easy to back this up with studies. Most studies are expensive because you try to show how a treatment is working better than a placebo. But showing that most people with reflux have low stomach acid? That would not be a big deal. The low stomach acid theory also contradicts the experience of other experts in the field, like Dr. Jamie Koufman who writes about the low acidity myth in one of her books.
By the way: I tried to get Dr. Wright for an interview to discuss his book, but he declined.
The book has great reviews. However, if you read through his books reviews on Amazon, you will realize: most people reviewed after they read the book but before they tried the treatment. People just found the book a very interesting read. Few wrote which benefits they got from the recommendations.
In his defense: the book is actually not about reflux. Dr. Wright also does not claim to be a reflux expert. Instead, he tries to explain how the digestive tract works and how you can improve digestion with different natural remedies. In that regard, his book is very interesting. He makes a case against long term usage of acid-reducing medication.
However, what people remember is that he can supposedly cure pretty much everybody of reflux by supplementing with stomach acid and digestive enzymes. Reflux is a complex disease. I can absolutely believe that this works for a small percentage of people, but not even close to everybody.
Dr. Wright claims that boosting acid and digestive enzymes works for most of his patients. I do not want to say he is a liar. Maybe people who are proven to have low stomach acid are simply actively looking for his help. What might work for this sub-group of people will not work for the general population.
If low stomach acid were the cause for reflux, then the rebound effect from PPI usage would not exist. We discussed the rebound effect above - increased reflux symptoms after stopping acid blockers. The rebound effect is caused because your acid production is higher than normal for a while. The effect is the same as supplementing with acid. If the claims of the book were true, increased acid production from stopping PPIs should heal reflux for a while – not worsen it.
You only need to remember one thing from the last few paragraphs. If someone claims that supplementing stomach acid can cure reflux in everybody: do not believe that statement easily. It might be true for a small percentage of people, but not for most.
5. Small Intestinal Bacterial Overgrowth
There is another topic which got a lot of buzz in recent years: small intestinal bacterial overgrowth (SIBO).
SIBO means that harmful bacteria have spread into and overgrown the small intestines. In simpler terms: the gut flora is out of balance.

These bacteria digest parts of our food and at the same time produce gas. This can reduce the effectiveness and general health of your digestive system.
In his book "The Fast Track Diet", Norm Robillard describes why he sees SIBO as an important cause of reflux. The bacteria produce gas which then pressurizes or leaks into the stomach. This increase in pressure causes reflux.
Robillard recommends avoiding foods that nourish the bad type of bacteria in the intestines. Those bacteria thrive on fermentable carbohydrates like sugar, grains, fiber & fructose. Most legumes like beans and peas are also highly fermentable and worsen SIBO.
SIBO has once been described as “quack” or pseudo-science. But LPR research started the same way. Today more and more diseases are being linked to SIBO, and it is becoming an accepted concept in the medical community.
Whether SIBO is related to LPR is still a polarizing question. It is worth testing whether an anti-SIBO diet helps you. Note that many SIBO diets tend do be overly complicated and confusing. The book linked above is the only one I can recommend at this point.
Foods with a low fermentation potential from the book can be combined with a low acid diet. It avoids reactivation of pepsin. Most acidic fruits contain fermentable sugars anyway.
One word of caution: only for a small percentage of people, SIBO is the cause of their reflux. It was a tough decision whether I should even recommend the above book. What raised a huge red flag for me is that the author praises his method as being the ultimate cure against any kind of reflux (and many other diseases). He turns down widely and scientifically proven causes of reflux as lies without backing that up in any way.
It is a classic approach for selling treatments that are based on the placebo effect. The more you make people believe in a method, the stronger the placebo effect is. Still, a small number of people will profit from an anti-SIBO diet.
However, do not take all of the information in the book as absolutely true. I also do not recommend an anti-SIBO diet as a primary treatment, only as something to try out if you do not get relief from other strategies.
Treatment Options are Plentiful
There are many possible causes for LPR and therefore at least as many potential solutions.
Are you confused where to start? Click here to check out my online course on curing LPR. In the course, multiple proven experts will tell you how to fix your symptoms. It will speed up your recovery. You will avoid making treatment mistakes that only make your symptoms worse.
Most LPR patients are treated completely wrong. Many physicians put their patients on PPIs, give some basic diet advice, and that's it. Most people still have LPR symptoms afterward. They are told by their physicians that there is nothing else to do. No wonder many become frustrated or even depressed.
You shouldn’t be. In the doctor's office, there is rarely more time than to prescribe a pill.
There are many possible treatments for LPR out there.
Become the advocate of your own health, and you will cure your LPR.


About the Author
Gerrit Sonnabend
Gerrit is a German data scientist & medical publisher. His formal education is in qualitative research. He had severe reflux himself.